November 09, 2021
How smarter decisions reduce employee healthcare benefits costs

Heidi Pearson
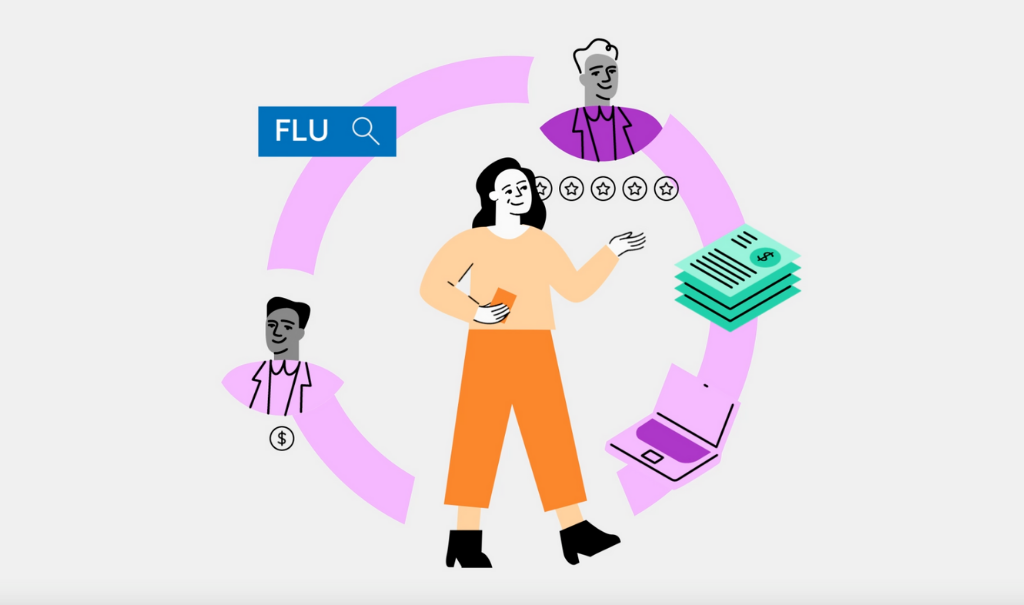
Guiding employees to smarter healthcare choices year-round can reduce claims and benefits costs while improving care quality.
Self-insured employers may differ in size and benefits design approaches, but they all share a common healthcare goal: Provide a competitive employee benefits package while controlling rising costs for their plans. This year, healthcare costs are an even bigger priority than usual. Harvard Business Review reports that health insurance costs for employers are expected to rise in 2022, projecting that nationally, premiums will increase over 5%. This increase—combined with overall market uncertainty related to COVID-19 and the impact of deferred care in 2020 and 2021—can make quick cost reduction measures seem appealing. Some employers may choose to raise copayments and deductibles for employees. Others may roll out new health and wellness programs to support employees with high-cost conditions. And a subset may cut benefits altogether to offset other expenses.
While these approaches can help reduce benefits costs short-term, they don’t address an important long-term factor contributing to rising costs: Variation in healthcare prices and quality. In every network, there are providers who deliver great care at efficient prices, and there are providers who deliver inappropriate, wasteful, or unnecessarily expensive care. The problem is, it’s almost impossible for your plan or your members to know which providers are high quality and lower cost and which ones aren’t. As a result, everyone pays more for healthcare without getting consistent value.
While short-term benefits changes may be necessary this year, it’s important to lay the groundwork for long-term program improvements as well. Investing in a healthcare guidance solution that helps your employees find the best providers in your existing networks is a great way to make a positive, lasting impact on both your employees’ health and your company’s healthcare benefits spend. When your plan members consistently choose high-value options for all their care needs—whether it’s a simple PCP or pediatrician visit or a complex inpatient surgery—both they and your health plan will see a significant reduction in healthcare costs.
The impact of convenient, data-driven healthcare cost guidance
Healthcare guidance solutions can be a powerful way to direct your members to the high-value corners of your existing networks, without requiring any plan design changes. Amino’s digital care guidance solution clients achieve healthcare cost savings in four important ways:
- Reduced out-of-network (OON) visits. OON claims account for 18% of inpatient admissions and 8% of outpatient admissions for employer health plans. That’s because many people don’t understand which doctors and facilities are covered by their plan’s network and which ones aren’t. Even using a carrier provider directory to search for doctors can lead to accidental OON bills because of data inaccuracies. Amino’s Find Care search experience displays only in-network providers by default and uses a two-step verification process during appointment booking to help employees get care from providers covered by their plan. On average, employers see OON costs decrease by approximately 30% when their members use Amino to find care options.
- Reduced utilization of high-cost, low-quality healthcare providers. While healthcare cost and quality data is useful, most people don’t have the time or interest to sift through tons of stats when choosing a doctor or facility. Amino’s Smart Match recommendations use all this data to point plan members toward the best providers for their personal health needs based on three criteria: network status, cost of services and procedures, and care quality and experience. When employees choose a Smart Match provider, they can count on getting high-quality care at a lower cost—anywhere between $100 for a primary care visit and $11,000 for an inpatient stay. That adds up to measurable savings for benefits programs over the course of a plan year.
- Increased use of employer-sponsored healthcare benefits at the right time. Many HR teams invest a lot time and money into developing a generous benefits package that only a small percentage of employees ever use. Amino integrates healthcare benefits such as telemedicine, direct primary care, chronic condition management apps, and other offerings in search results so employees find the right solution when they need it most. This convenient and timely way of displaying benefits drives increased utilization—and ultimately, healthcare cost savings. For example, if your company offers a digital mental health service, Amino will tag this benefit to related search terms in the platform. When an employee searches for a health need like “major depression” or “bipolar disorder,” they’ll see your benefit included in search results, in addition to appropriate in-network providers. Amino tracks activity on these benefits so you can see how many people click through to another service every month and understand which offerings provide the most value.
- More care received in appropriate healthcare settings. One of the most challenging parts about navigating the U.S. healthcare system is knowing where to get care—especially for acute health issues. The NEHI found that ER overuse contributes $38 billion to wasteful healthcare spending each year. But expecting employees to weigh the pros and cons of calling their PCP versus heading to the nearest ER when they (or a family member) are having a significant health issue isn’t realistic. Amino makes it easy for employees to get the right care from the right kind of provider with a jargon-free search experience and Smart Match recommendations. In less than 30 seconds, members can find an appropriate place to get treated—without needing to be healthcare experts.
Choosing a healthcare guidance partner
There are a variety of different healthcare guidance options available to employers. Here are some important factors to consider as you shop around for the right solution:
Customization
The most helpful healthcare recommendations are personalized to an individual member’s plan design, health needs, and preferences. Avoid solutions that use a one-size-fits-all approach to care guidance. Amino works closely with employers to tailor its search and booking experience to specific plan designs (PPO/EPO/RBP/Tiered), carrier networks, and sponsored health benefits. Amino also supports single sign-on (SSO) integration so employees can access the platform from your company’s existing health benefits systems.
Implementation
The sooner employees can start using a healthcare guidance solution, the sooner your company will start seeing bottom-line results. Launch timelines can vary drastically by vendor depending on their implementation approach. Standard implementations with Amino take just 4-6 weeks, but other organizations may require months of lead time. Ask potential solutions providers about their onboarding and account setup process to understand how quickly employees can start using the platform.
Customer support and account management
What happens after your team implements a new solution? Will you receive the support you need to onboard employees and work through any rollout hiccups? Will your employees have access to timely support if they have questions or need help? And will there be someone to guide your program’s strategic approach to healthcare benefits so you continue to provide value to your organization? Whatever solution you choose, make sure your HR team and your employees will receive reliable support and account management services. With Amino, clients receive a dedicated customer success manager to help with account needs, engagement materials and strategies, analytics reviews, and plan/benefit updates. We also provide flexible member support via phone and our online help center.
Reporting
When you’re evaluating the impact of your chosen healthcare guidance solution, you need ongoing metrics to understand how members are engaging and what savings the platform is driving for your program. Amino will send you monthly insights reports that track member engagement (logins, searches, bookings), most commonly searched healthcare topics, cost savings opportunities, and other helpful information.
The healthcare landscape is complex and ever-changing. By investing in a healthcare guidance solution, you can save your program money—and improve your members’ healthcare experience and outcomes—both now and in the future.
Connect with our Partnership Team
Want to learn how we can help your members transform their healthcare experience in 2025?